HEALTH
Understanding Sciatica: When an MRI Is Necessary for Treatment

Sciatica is a condition that can cause severe pain, often radiating from the lower back down to one or both legs. It’s a common ailment, but the treatment options vary depending on the underlying cause. While many people find relief from conservative treatments like physical therapy or medication, some cases require more extensive evaluation. One tool that plays a crucial role in diagnosing and managing sciatica is magnetic resonance imaging (MRI). In this article, we’ll explore when an MRI is necessary for treating sciatica and how it can provide essential insights into the condition.
What Is Sciatica?
Sciatica refers to pain that travels along the sciatic nerve, which runs from your lower back, through your hips and buttocks, and down each leg. It is not a condition itself but rather a symptom of an underlying issue, often related to nerve compression. The pain is typically one-sided and can vary from mild discomfort to debilitating agony.
The most common causes of sciatica include a herniated disc, spinal stenosis, or degenerative disc disease. These issues can put pressure on the sciatic nerve, causing inflammation, pain, and sometimes numbness or tingling sensations in the affected leg. Other factors, such as muscle imbalances or piriformis syndrome, can also contribute to sciatica.
If you are experiencing symptoms such as sharp, shooting pain, or a constant ache that affects your ability to walk or sit comfortably, it’s essential to consult a healthcare provider. If you’re unsure about your symptoms, you can learn more about Sciatica at Modern Orthopaedics, where experts offer comprehensive care and treatment plans for sciatica and related conditions.
The Role of MRI in Diagnosing Sciatica
MRI, or magnetic resonance imaging, is a non-invasive imaging technique that uses powerful magnets and radio waves to create detailed images of the internal structures of your body. Unlike X-rays, which primarily show bone structures, MRIs are excellent for examining soft tissues such as muscles, nerves, and discs.
In the case of sciatica, an MRI is a crucial diagnostic tool because it can reveal the underlying causes of nerve compression. For example, a herniated disc may be pressing on the sciatic nerve, which could be the source of the pain. Spinal stenosis, or narrowing of the spinal canal, is another condition that can be diagnosed using MRI and may contribute to sciatica. The detailed images produced by an MRI allow doctors to assess the severity of the problem and determine the best course of treatment.
One of the key advantages of MRI over other imaging techniques is its ability to provide detailed images of soft tissues. For example, it can help doctors identify bulging or ruptured discs, misalignments, or other abnormalities that an X-ray would miss. This is why MRIs are often the preferred diagnostic tool when sciatica symptoms are severe or persistent.
When Is an MRI Necessary for Sciatica Treatment?
Not all cases of sciatica require an MRI. In fact, most sciatica symptoms resolve on their own with conservative treatments like rest, physical therapy, or over-the-counter pain relievers. However, there are certain situations where an MRI becomes necessary for proper diagnosis and treatment.
1. Persistent or Severe Symptoms
If your sciatica symptoms have lasted for more than 4-6 weeks and don’t improve with conservative treatments, it may be time for an MRI. Chronic pain or significant discomfort that interferes with daily activities could indicate an underlying issue that requires further investigation. An MRI can provide a clearer picture of what is causing the pain and help determine whether more aggressive treatments are necessary.
2. Severe or Progressive Symptoms
Certain signs may indicate that the situation is more serious and requires immediate attention. For example, if you experience leg weakness, difficulty controlling bladder or bowel functions, or significant pain that radiates down one leg, an MRI may be necessary. These symptoms could indicate a more severe nerve compression or even a herniated disc that is putting pressure on the spinal cord. An MRI can help identify these issues and guide the treatment plan.
3. To Rule Out Other Conditions
In some cases, sciatica-like symptoms may be caused by other underlying conditions such as infections, tumors, or fractures. An MRI is a useful tool for ruling out these possibilities, as it provides a detailed image of the spine and surrounding structures. If your doctor suspects that something other than a simple disc herniation may be causing your sciatica, they may recommend an MRI for further investigation.
4. Failure of Conservative Treatments
If your sciatica symptoms do not improve after several weeks of conservative treatments, an MRI may be needed to evaluate whether surgery or other invasive treatments are required. MRI results can help doctors assess the extent of nerve damage or disc issues, which can influence whether surgery or other interventions are necessary.
What an MRI Can Reveal About Sciatica
An MRI can uncover a variety of conditions that may be contributing to sciatica. Here are some of the most common findings:
- Herniated Discs: One of the most common causes of sciatica, herniated discs occur when the soft inner material of a spinal disc pushes through the outer layer and compresses nearby nerves. An MRI can reveal the location and extent of the herniation.
- Spinal Stenosis: This condition involves the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves. MRI scans can show areas of narrowing, helping doctors determine the best treatment approach.
- Degenerative Disc Disease: Over time, spinal discs can wear down and lose their cushioning ability. MRI can identify these degenerative changes and their impact on nearby nerves.
- Spondylolisthesis: This occurs when one vertebra slips out of alignment over the one below it, often leading to nerve compression. MRI can detect this misalignment and help doctors plan the appropriate treatment.
- Tumors or Infections: In rare cases, tumors or infections can cause sciatica-like symptoms. An MRI is essential for detecting these serious conditions and differentiating them from more common causes of sciatica.
If you’re in New Jersey and want to better understand your MRI results or discuss treatment options, you can request an MRI review in New Jersey with a local healthcare provider like those in New Jersey Spine Institute.
Alternatives to MRI in Sciatica Diagnosis
While MRIs are invaluable in diagnosing sciatica, they are not always the first step in treatment. In many cases, a doctor will perform a physical examination and may recommend other diagnostic tests, such as X-rays or CT scans.
X-rays can show bony abnormalities, such as bone spurs or fractures, but they cannot provide detailed images of soft tissues like nerves and discs. CT scans, which use a series of X-rays to create cross-sectional images of the body, can offer more detail than a traditional X-ray and may be used in place of an MRI if needed.
Nerve conduction studies and electromyography (EMG) tests may also be used to evaluate the function of the nerves and muscles, especially if there is concern about nerve damage.
Conclusion
MRI plays a vital role in diagnosing sciatica and guiding treatment decisions. For most people, sciatica improves with conservative treatments, but if the pain is severe, persistent, or associated with other concerning symptoms, an MRI can provide valuable insight into the underlying cause. Whether it’s identifying a herniated disc, ruling out more serious conditions, or helping determine the need for surgery, MRI scans are an essential part of the sciatica treatment process. If you’re struggling with sciatica, it’s important to consult with a healthcare provider to determine whether an MRI is necessary for your diagnosis and treatment plan.
HEALTH
Essential Considerations After a Personal Injury Incident

What to Do Immediately After an Incident
A personal injury incident can strike unexpectedly, leaving you feeling disoriented and vulnerable. In these crucial moments, your priority should be ensuring everyone’s safety, including yours. Begin by assessing the environment for hazards such as traffic, unstable structures, or exposed electrical elements. If necessary, quickly move to a safe location or, if incapacitated, signal for help.
Once safety has been established, it is essential to maintain a sense of calm. While this is challenging, keeping a clear mindset enables sound decisions. You may already consider the potential legal ramifications and wonder about personal injury law during this time. This understanding is crucial as it informs how you handle the initial stages after an injury.
Understanding Your Rights
Understanding your rights following a personal injury can be a source of empowerment. Individuals affected by such incidents frequently encounter many decisions, ranging from medical care to possible legal recourse. Typically, victims have the right to seek compensation for their injuries, which may encompass physical damage, emotional suffering, and financial setbacks, including lost wages or medical expenses. Engaging a personal injury lawyer can facilitate obtaining the compensation you are entitled to, as they can assist in navigating the legal complexities on your behalf. Having a well-informed strategy can significantly impact the outcome of any legal matter. To enhance your understanding, explore comprehensive resources that explain your legal rights as an injury victim.
Gathering Necessary Evidence
The strength of your compensation claim hinges significantly on the evidence gathered at the scene. Documenting the scene might seem challenging in the chaotic aftermath of an accident, but it is a vital step. Take clear photographs from multiple angles, capturing details like road conditions or visible injuries.
Should witnesses be available, collect their contact details and courteously request their event description. Written statements or voice recordings are invaluable. Secure any video footage from nearby cameras, such as traffic or security cameras, which could provide an unbiased account of the incident.
Seeking Medical Attention
Medical attention should be sought immediately after ensuring safety, even if injuries appear to be minor. Prompt medical evaluations are necessary for your health and serve as critical evidence. Minor aches or bruises indicate underlying injuries that could have been left unchecked.
A detailed medical report is an official record of your injuries and is often crucial when filing compensation claims. For instance, understanding the importance of medical procedures like X-rays can better illustrate how injuries are documented and assessed. Skipping this step can lead to complications in your recovery and legal proceedings.
Reporting the Incident
Once immediate concerns are managed, you should report the incident to the authorities. This includes contacting the police to file an official report. This report creates an official and unbiased account of what transpired, which lawyers and insurance companies often examine closely.
Be honest and concise in your account to the authorities. Provide them with the collected evidence, but refrain from speculating about fault or liability, as emotions and stress can colour your perspective.
Consulting a Professional
Personal injury cases often present complexities and involve nuanced details requiring expert guidance. Engaging a personal injury attorney can offer valuable clarity and assistance. A lawyer represents your interests and expertlymanoeuvress through the intricacies of the legal system on your behalf, guaranteeing that you obtain the compensation to which you are entitled.
Prepare for these consultations by gathering all relevant documents. Questions to discuss include your case’s strengths and the lawyer’s experience with similar claims. This relationship will be instrumental, so choose a lawyer whose communication style you find agreeable and who clearly outlines their strategy and expectations.
Navigating Insurance Claims
Filing an insurance claim demands patience and precision. Write down all correspondence with the insurance company and keep detailed records of every exchange. Respond promptly to communications and provide all requested documentation, including medical reports and evidence collected at the scene.
Insurance companies aim to minimize payouts, so be prepared to advocate for yourself firmly. Proactively engaging in the process with a straightforward narrative supported by evidence builds a compelling case for a fair settlement. Avoid rushing the process; thoroughness now can prevent complications later.
Staying Informed and Educated
Finally, education is an ongoing process that bolsters your readiness for personal injury incidents. Continuously familiarize yourself with personal injury law as it evolves with new precedents and legislative changes. This knowledge assists you in the immediate aftermath of an incident and prepares you for potential future scenarios.
Explore readings from reputable legal sources, attend workshops, or consult experts to enhance your understanding. Being well-informed isn’t just about being prepared—it’s about staying empowered in all legal and personal protection aspects.
HEALTH
Factors That Affect Breast Implant Prices in Baton Rouge
Choosing to undergo breast augmentation is a significant decision, and understanding the cost is essential for making an informed choice. The price of breast implants can differ depending on factors influencing the overall cost. For those considering this procedure, it’s essential to understand what affects the price.
In Baton Rouge, breast implant costs vary greatly based on multiple factors. From the surgeon’s experience to the type of implants, every element contributes to the final price of the procedure. When considering a procedure, it’s essential to research about the breast implants Baton Rouge price to ensure it aligns with your budget and expectations.
Surgeon’s Experience and Reputation
One of the most significant factors determining the price of breast implants is the surgeon’s experience and reputation. Due to their expertise, experienced, board-certified surgeons specializing in breast augmentation often charge more. They provide a higher level of care, and their track record of successful surgeries justifies the cost. While opting for a more affordable surgeon might seem appealing, the quality and safety of the surgery should be the priority. An experienced surgeon in Baton Rouge ensures the best results, making the investment worthwhile in the long run.
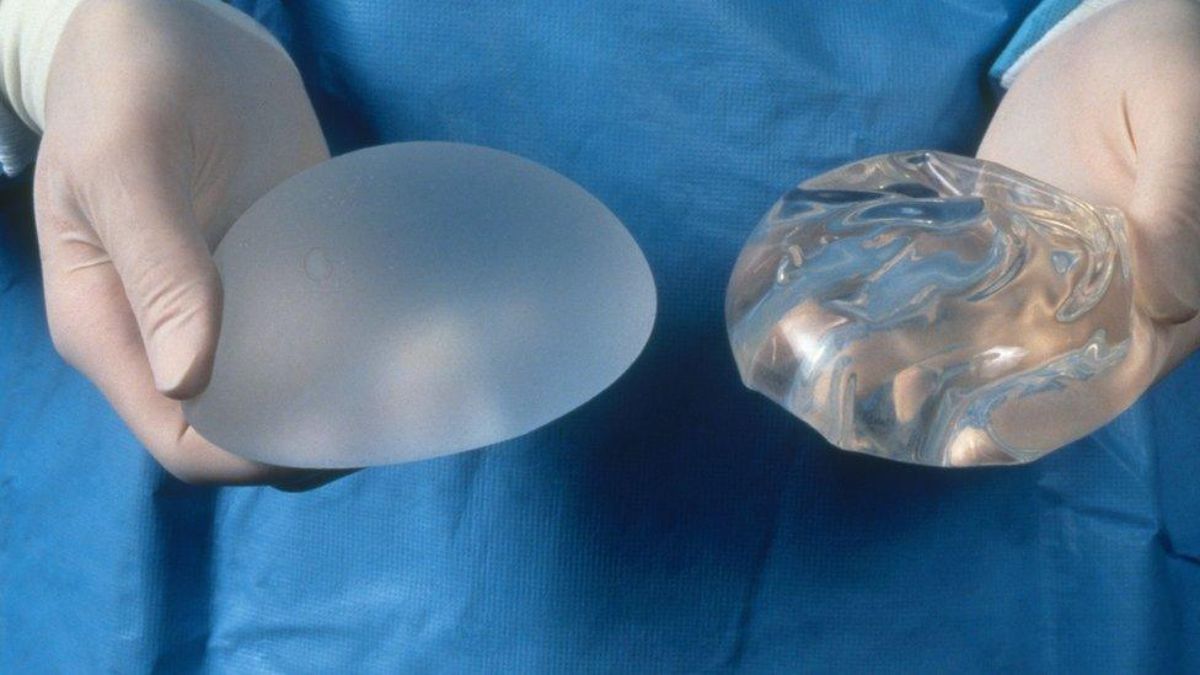
Type of Implants Chosen
The type of implants chosen by the patient significantly impacts the overall cost. Saline implants are typically more affordable than silicone implants, which are more expensive due to their construction and natural feel. Patients can also choose between textured or smooth implants, which may cost differently. The decision on implant type depends on factors like desired aesthetic results and personal budget. A consultation with a qualified surgeon in Baton Rouge will help patients decide which implant best suits their body and goals while also considering the cost.
Location and Market Factors
Local market conditions can also influence the cost of breast implants in Baton Rouge. Prices can vary depending on the demand for cosmetic surgery in the area and the number of qualified surgeons available. In areas with higher demand for breast augmentation, the cost may increase. The local cost of living and the reputation of specific clinics can also affect pricing. Patients should research local clinics and compare prices while keeping in mind that the quality of care and expertise should not be compromised for a lower price.
Facility and Anesthesia Fees
The surgical facility and anesthesia fees are important factors in the overall price. The location of the surgery center, whether it’s an outpatient clinic or a hospital, can affect the cost. Some clinics charge higher fees for their facilities, which may include more advanced equipment and higher standards of care. Additionally, anesthesia fees vary depending on whether general or local anesthesia is required. General anesthesia tends to be more expensive than local anesthesia. Patients should ask for a detailed breakdown of all these costs during the consultation to ensure they fully understand the price.
Additional Considerations When Seeking Breast Implants
When considering breast augmentation, finding a provider that offers personalized care throughout the entire process is essential. Many clinics provide detailed consultations where patients can discuss their goals, review different implant options, and receive advice tailored to their needs. These consultations help patients understand the costs and the level of care they can expect. By choosing a clinic in Baton Rouge that emphasizes patient satisfaction and safety, individuals can ensure a smoother and more successful experience.
Breast implants Baton Rouge price can vary based on factors such as the surgeon’s experience, the type of implants selected, the complexity of the procedure, and associated facility and anesthesia fees. Understanding these elements helps patients plan financially and choose the correct option. By consulting with a reputable surgeon, prospective patients can ensure they receive the best value for their investment while achieving their desired results.
HEALTH
Stress and Ovarian Cysts: Can Anxiety Make Your Symptoms Worse?

When dealing with ovarian cysts, the physical symptoms—like pelvic pain, bloating, and irregular periods—can be overwhelming enough on their own. However, for many women, the emotional and psychological aspects of living with ovarian cysts are just as significant. One factor that often exacerbates these symptoms is stress.
But how exactly does stress affect ovarian cysts, and can anxiety make your symptoms worse? In this blog, we’ll explore the intricate relationship between stress and ovarian cysts, how stress might impact the severity of your ovarian cyst symptoms, and what you can do to manage both the physical and emotional aspects of dealing with ovarian cysts.
What Are Ovarian Cysts?
Before diving into how stress and anxiety can affect ovarian cysts, it’s important to understand what they are. Ovarian cysts are fluid-filled sacs that develop on or inside the ovaries. They are relatively common, especially in women of reproductive age, and most ovarian cysts are benign (non-cancerous). Many women experience no symptoms at all, while others may have pain or discomfort.
There are several types of ovarian cysts, with the most common being functional cysts, which occur during the menstrual cycle. These cysts usually resolve on their own without treatment. However, some women may experience more complex cysts that can cause symptoms like:
- Pelvic or abdominal pain
- Bloating
- Irregular or heavy periods
- Pain during sex
- Nausea or vomiting
While most cysts are harmless and go away on their own, some can grow, cause complications, or affect fertility. For women experiencing persistent symptoms, stress can be both a contributing factor and a result of dealing with a chronic condition like ovarian cysts.
The Link Between Stress and Ovarian Cysts
Stress is an inevitable part of life, but when it becomes chronic, it can have a profound impact on your physical health, including your reproductive system. Research shows that stress affects the body in many ways, from disrupting hormone levels to causing inflammation, both of which can influence the formation or worsening of ovarian cysts.
Here’s how stress might contribute to or worsen ovarian cyst symptoms:
Hormonal Imbalance
Stress triggers the release of the “stress hormone” cortisol. Cortisol is part of the body’s natural fight-or-flight response, which is essential for managing acute stress. However, prolonged stress can lead to consistently high cortisol levels, which may disrupt the delicate balance of other hormones involved in the menstrual cycle, such as estrogen and progesterone.
An imbalance in these hormones can have a direct effect on ovarian function. For example, high cortisol levels may prevent the proper release of eggs from the ovaries, a process known as ovulation. Without proper ovulation, the ovarian follicle can become a cyst. Additionally, hormonal imbalances can cause irregular periods, which may make cysts more likely to form or grow.
Increased Inflammation
Chronic stress also triggers the body’s inflammatory response. Inflammation can interfere with normal bodily functions, including those of the reproductive system. Inflammation may cause the ovaries to become more susceptible to cyst formation or exacerbate the symptoms of existing cysts, leading to increased pain, bloating, or discomfort.
In some cases, inflammation may lead to more serious complications, such as the rupture of a cyst, which can result in severe pain and, in rare cases, infection.
Muscle Tension and Pain Perception
When stressed or anxious, the body tends to tense up, particularly around the shoulders, neck, and abdominal area. This muscle tension can increase pelvic discomfort in women with ovarian cysts. The sensation of pain or pressure caused by a cyst may feel more intense when your muscles are tight and stressed.
In addition, stress can alter your perception of pain, making you more sensitive to discomfort. This means that the pain from a small ovarian cyst might feel much worse when you’re under stress or anxious. This can create a cycle where anxiety about the cyst causes more stress, which in turn makes the pain feel more unbearable.
Gut and Digestive Issues
Stress can also have a significant impact on the digestive system. Anxiety and stress can lead to issues like bloating, constipation, and stomach cramps—symptoms that overlap with the symptoms of ovarian cysts. When you’re already dealing with abdominal discomfort due to a cyst, additional digestive problems caused by stress can make everything feel worse.
Furthermore, chronic stress can lead to conditions like irritable bowel syndrome (IBS), which may increase bloating and digestive distress, further exacerbating the discomfort associated with ovarian cysts.
Reduced Immune Function
Stress has a detrimental effect on the immune system. Prolonged stress can weaken immune function, making the body less able to deal with infections or inflammation. This can affect your ovaries, increasing the likelihood of complications such as cyst rupture or infection. Additionally, a weakened immune system may delay the healing of cysts or prolong the symptoms associated with them.
How Anxiety Can Impact Ovarian Cyst Symptoms
Anxiety, which often accompanies stress, can also play a major role in exacerbating ovarian cyst symptoms. Anxiety causes the body to stay in a heightened state of alert, activating the fight-or-flight response even when there is no immediate danger. This prolonged state of arousal can lead to physical changes in the body that make ovarian cyst symptoms worse.
Some specific ways anxiety can affect ovarian cysts include:
- Hypervigilance about symptoms: When you’re anxious, you may become hyper-aware of any sensations in your body. This can cause you to focus excessively on your ovarian cyst symptoms, making them seem worse than they are. This heightened awareness can also lead to unnecessary worry and stress.
- Sleep disturbances: Anxiety can interfere with your ability to sleep, leading to fatigue and an overall decrease in your ability to cope with physical symptoms. Poor sleep can also increase your sensitivity to pain, making the discomfort from ovarian cysts more difficult to manage.
- Behavioral effects: Anxiety can lead to unhealthy coping mechanisms, such as overeating or drinking alcohol, which can worsen inflammation and disrupt hormone balance, potentially making ovarian cysts more problematic.
Managing Stress and Anxiety to Relieve Ovarian Cyst Symptoms
Given the connection between stress, anxiety, and ovarian cysts, managing your emotional well-being is crucial for alleviating symptoms. Here are several strategies you can incorporate into your daily routine to help reduce stress and anxiety:
Practice Mindfulness and Meditation
Mindfulness practices, such as meditation and deep breathing exercises, can help calm your nervous system, reduce cortisol levels, and ease physical tension. Even just 10–15 minutes of mindfulness a day can help regulate your stress levels and improve your overall sense of well-being.
Exercise Regularly
Exercise is a powerful tool for stress reduction. Physical activity helps release endorphins, which are natural mood boosters, and can also help improve sleep quality and reduce anxiety. Aim for activities you enjoy, such as walking, swimming, or yoga, which can also alleviate muscle tension and promote relaxation.
Manage Your Diet
A balanced diet can play a role in reducing stress and supporting your reproductive health. Foods rich in antioxidants, omega-3 fatty acids, and fiber can help reduce inflammation and support hormonal balance. Limiting caffeine and alcohol intake can also help stabilize your mood and energy levels.
Therapy and Counseling
If anxiety is affecting your daily life, talking to a therapist can be beneficial. Cognitive-behavioral therapy (CBT) is particularly effective for anxiety and stress management. A mental health professional can help you develop coping strategies and reduce anxiety related to your cyst symptoms.
Stay Connected with Support Networks
Talking to friends, family, or others who are going through similar experiences can provide emotional relief. Support groups, whether in-person or online, can be a great way to share your concerns, receive advice, and feel understood.
Seek Medical Advice
If you’re experiencing significant pain or discomfort from ovarian cysts, it’s essential to speak with a healthcare provider. They can provide treatment options, including medication for pain management or hormonal regulation. In some cases, they may recommend surgery to remove the cyst, especially if it is causing severe symptoms.
Conclusion
Stress and anxiety can significantly impact the severity of ovarian cyst symptoms, from hormonal imbalances to increased pain and digestive issues. While it may not be possible to completely eliminate stress from your life, managing it effectively can help reduce the physical and emotional burden of dealing with ovarian cysts. By incorporating stress-reduction techniques like exercise, mindfulness, and proper medical care, you can help improve your overall health and minimize the impact of ovarian cysts on your life.
If you’re struggling with symptoms of ovarian cysts or experiencing heightened anxiety, don’t hesitate to consult with a healthcare provider. Together, you can develop a comprehensive plan to manage both your physical and emotional well-being.
-

 TECHNOLOGY7 months ago
TECHNOLOGY7 months agoAbout Technology From Axiumtechnet: Exploring the Beautiful Future
-

 TOPIC6 months ago
TOPIC6 months agoInvitation Printing: How to Create Perfect Invitations for Any Occasion
-

 TECHNOLOGY6 months ago
TECHNOLOGY6 months agoThe Rise of Hqpotner: Exploring Its Impact on the Blogging Community
-

 TECHNOLOGY7 months ago
TECHNOLOGY7 months agoAlpha Technologies Fxm350 Snmp Oid: Comprehensive Overview
-

 BUSINESS7 months ago
BUSINESS7 months agoGoogle Business Profile Kgmid Extractor: A Deep Dive
-

 HEALTH7 months ago
HEALTH7 months agoHarriet Goldfischer Providence Health: Ultimate Guide
-

 BUSINESS6 months ago
BUSINESS6 months ago36dview Photography Business Info: Your Ultimate Guide
-

 BUSINESS7 months ago
BUSINESS7 months agoDining Delights: 200 E Business Hwy 23 Walsco Tx
